Ken Newell
Serving your community as a firefighter has always been recognized as a dangerous, yet rewarding endeavor. Most of the dangers have been fairly easy to identify. Line of duty injuries or deaths have resulted from several sources including structure fires, automobile accidents, heart attacks, and high blood pressure.
Serving your community as a firefighter has always been recognized as a dangerous, yet rewarding endeavor. Most of the dangers have been fairly easy to identify. Line of duty
injuries or deaths have resulted from several sources including structure fires, automobile accidents, heart attacks, and high blood pressure. Because of these events and ailments, firefighters typically pay higher life and health insurance rates than the average person.
But over the past couple of decades, a silent killer is growing exponentially in this
profession.
The Challenge - Cancer.
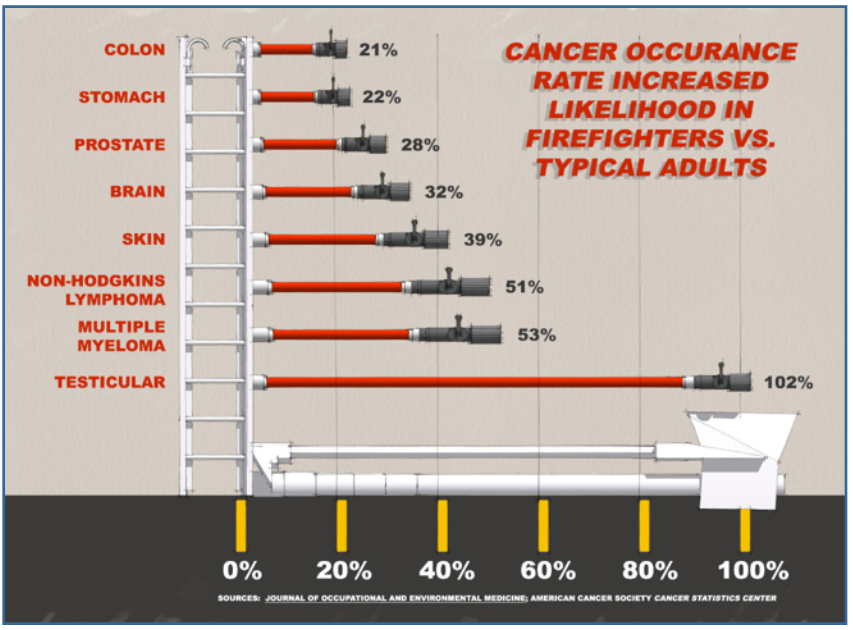
We’re a public safety design firm well into our fifth decade of working with fire departments. Unfortunately, over the past twenty years, we’ve watched the number of fire-fighting friends that have been impacted by cancer greatly increase. A rural VFD in Virginia that we are working with illustrates this point, and serves as an example of what many departments are facing. Over the past two years, this thirty-member Volunteer Department has had four members battling cancer. That’s nearly 15% of the members. In fact, according to both the Journal of Occupational and Environmental Medicine and the American Cancer Society Cancer Statistics Center, across eight of the most commonly diagnosed cancer types - on average - firefighters are 43% more likely than the general population to develop cancer. These eight types of cancer are colon, stomach, brain,
testicular, skin, and prostate, myeloma, and Non Hodgkin’s lymphoma.
The Perpetrators
In order to better understand these staggering occurrence rates, we need to travel back to high school chemistry class and name the contaminants that are causing all this havoc. We’ll call these known carcinogens “the perpetrators”.
They include carbon monoxide, formaldehyde, butadiene, isocyanates, benzene, nickel, arsenic, nitrogen dioxide, acrylonitrile, toluene, and numerous other hydrocarbons. There are many other elements encountered at the fire- grounds, but these are some of the most recognized carcinogens. Even those of us not in the fire-fighting industry encounter these perpetrators from time to time and most of us don’t end up with cancer. The problem for first responders is the repeated cycle that they are exposed to for these carcinogens. First, they respond to a scene where these elements are present. They are exposed to them. Then the responder returns to the station, contaminating many items there and possibly at home. Then, with the next call, the cycle happens all over again, day after day. The fire ground and the rescue call can include dozens of sources of these dangerous elements. When you think about the materials contained in buildings, cars, and furnishings today – compared to fifty years ago - the dangers are easy to understand. Just the predominance of plastics in so many products today is mind boggling. So it’s not just a fire at a chemical plant that should concern us. Consider all the carcinogens listed above that are encountered in a house fire or a car fire. And the elements you will encounter “dumpster diving” to extinguish a dumpster fire can be nearly unlimited, and certainly unknown.
Plus, it doesn’t have to be just combusted particles specifically from a fire. We all remember the great white clouds of particles that swept across Manhattan on 9/ll. That dust included asbestos and many other known carcinogens. Most of these elements or particles are so microscopic that they are invisible to the human eye. The smoke particles that are seen are usually much larger than the most dangerous carcinogens. Because the
elements are largely unseen, necessary care to exposure is often not practiced. What you don’t see can kill you! And to the point of this discussion, many of these “perpetrators” are carried back to the fire house. There are three major methods how these contaminants enter the human body. They can be ingested, inhaled, or absorbed.
Ingestion is easy to imagine once you think about it. Ingestion simply means that the contaminants are carried via saliva or mucus to the digestive system. If food or beverages consumed at the fire ground has been exposed, then eating or drinking them will put the contaminants to your digestive system. Even if just the containers or wrappers are exposed, ingestion is highly likely. At prolonged events, such as a fire ground, rehab areas often provide food and beverage. But have the refreshments been exposed to contaminants? And how often have you just wiped the soot off of the water bottle before
taking a drink?
Inhalation would be the most recognized form of contamination, because we often see so much smoke on the scene, and it irritates the throat and eyes. With this method of
contamination, the elements enters the respiratory system through the nose or throat. It is often thought that the elements are eliminated through coughing, sneezing, or even swallowing. But the contaminants make their way into the lungs, which deliver them to the
heart and the rest of the body through the blood. But this is why you wear SCBA,
right? Doesn’t that solve the inhalation problem? Every second on the fire ground without the SCBA mask being worn is a second of exposure. Just because the responder is not in thick smoke does not mean the danger is past.
Until they are completely clear of the fire ground AND everything that was exposed at the fire ground, off- gassing of contaminants on the PPE and equipment is occurring and being inhaled. Even on scene rehab can be dangerous while wearing the exposed PPE. Skin absorption is the least suspected of the three methods of entry into the body. Many are surprised because most of the body is covered by PPE during the fire response. But while PPE does well at keeping flame and heat away from the body, it still allows a great deal of smoke and particles on to the skin, thus absorption. Studies reveal that every place on the body where different articles of clothing interface, there are higher levels of smoke contamination. Once these contaminants are on the skin, they can be absorbed into the body and bloodstream. Making absorption more troublesome are the statistics showing that for every five degrees in human skin temperature the absorption of carcinogens through the skin increases by 400%.
The Station Culprits
So how do the fire ground perpetrators become the fire house culprits? Let’s consider how the contaminants are either transported to the station from the fire ground, or even how some contaminants are generated at the station PPE that has been exposed to carcinogens is commonly introduced back into the station. Most methods of decontamination used on PPE today still results in some level of off-gassing for hours, if not....
days. So wherever used PPE is stored in the station, there will likely be some level of contamination. The exterior AND interior of the apparatus returning to the station has likely been exposed to dangerous contaminants. While most departments do an
excellent job of keeping the apparatus clean, complete decontamination of these carcinogens is very difficult and rare. Think of all the equipment housed on and in your
apparatus. It is easy to understand how the items that were actually used during the response could have been exposed to contaminants, but even the items that stayed packed away on scene could be exposed. Much attention is often given to the decontamination of PPE, but how often are portable radios, tripods, or hose given
decontamination attention? Air packs and helmets get just as contaminated as PPE and require special attention for decontamination.
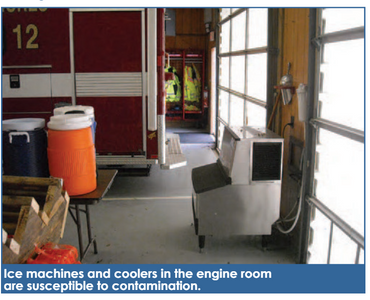
All of these items unaddressed, result in the cross contamination of air and elements in the station. The greatest station culprit that generates the contaminants is vehicle exhaust. Much has been discussed over the past few decades regarding fuel exhaust contaminants in the station and how it impacts PPE stored in the vehicle bays, but only recently has adequate attention been given to how these same carcinogens actually impact the human occupants in the facility. These indoor, running engines do more than just impact inhalation in the bays. Remember the other two means of contaminants entering the body? Ingestion and skin absorption. So vehicle exhaust inadequately addressed can lead to a wide range of potential contamination. It is very common to find ice machines in the vehicle bays. Reports show that OSHA has begun cracking down on this practice, and for good reason. The filtration system in an ice maker depends on the purity of the air being supplied to the machine. If the air around the ice maker contains contaminants, then the ice produced likely will as well, which can lead to eventual ingestion of the carcinogens. Vending machines in the vehicle bays also have a similar problem. The cans, bottles, or cartons inside the machine can be contaminated with exhaust fumes, which can lead to human ingestion and/or skin absorption. Laundry equipment exposed to exhaust contaminants is also in danger of producing contaminated “clean” laundry. One of the most beneficial trends in station design over the past few decades has been the inclusion of training props and opportunities. Many of these training opportunities occur in and around the vehicle bays. This important practice can result in two challenges to dangerous contamination. First, the props used for training are often items that have previously been exposed to contaminants and have not been adequately treated. Secondly, this training in the vehicle bays is an area or zone that contains and often generates its own dangerous contaminants.
The desire to perform rigorous decontamination and cleaning of equipment is often negated if the station does not have proper areas for the practice. If contaminated items are brought to the station kitchen sink for cleaning, all station personnel are in danger of ingesting and absorbing the contaminants when preparing and consuming meals later. Over the years, the vehicle bays of the station have been remembered fondly for all of the “nonapparatus” activities. It is rare to find a station over 10-20 years old that does not have some level of physical training occurring in the apparatus bays. Weights, exercise machines, basketball goals, crossfit equipment, etc., are all common sights in bays Ice machines and coolers in the engine room are susceptible to contamination.
across America. Departmental and community meetings, even bingo sessions are held in the apparatus bays regularly. Some departments still have operational watch desks or counters in the open vehicle bays. When the department has a station meal with a large group, it is often served in the vehicle bays. Very often open or unused areas of the vehicle bays accommodate seating, tables, even TVs, serving as a “secondary Dayroom” for station personnel. In light of the new recognition of carcinogens and their effect on fire fighters, providing space for all these activities away from the bays is even more important.
While we concentrate in this article on the constantly reoccurring exposure to fire fighters of carcinogens, there is also concern regarding unintended exposure to civilians at the station. Open house/tour days are a great way to show the community why the department is worthy of their support. But who has an open house or tour without taking the visitor through the highly contaminated apparatus bays? Many times refreshments, kids programs, even bands are set up in the bays.
Engine rooms still serve as polling places in many communities. Fundraising events and meals often utilize the very large, beneficial space found in the bays. Now that we have discussed the problem, the perpetrators, and the station culprits, let’s look at some opportunities for making a difference through the way that we think about the layout of a new or existing station.
Station Layout
First, let’s categorize the areas of the station based on their hazard. There are three major zones to the station. The Hot Zone is the high hazard or most contaminated area(s) of the station. This includes the apparatus bays and all areas that house or generate contaminants. The Cold Zone is the low hazard space(s). These are the areas where all
sources of the contaminants are to be kept out. This includes most of the living or human occupied portions of the station. The third zone is the Transition Zone. This is exactly what it sounds like - the real estate where you pass from Hot to Cold, and where you try to make impassible barriers to the contaminants. All properly designed or reconfigured stations will have the three zones occurring in the proper linear order: Hot to Transition to Cold, or Bays to Transition to Living Spaces. With this knowledge, consider your own station, or stations you’re familiar with. For example, the station with the apparatus bays in the middle, Administrative Spaces on one side of the bays, and living spaces on the other side of the bays… often referred to as a “saddlebag” stations… puts the Hot Zone in the center, with the Cold Zones on each side, with little to no Transition Zones. The occupants are constantly passing through the high hazard space to get to the other low hazard space.
Our goal here is to identify design strategies for making the station layout better, in regard to contaminants. These strategies fall into two major categories. First, we must contain the contaminants. Then, we must separate the facility occupants from the contaminants.
Since we have identified engine exhaust as the major contaminator from within, controlling exposure to diesel exhaust is a critical strategy. There are several methods for controlling diesel exhaust in the apparatus bays. Some of these include: filtration devices mounted to the apparatus engine, mechanical air evacuation systems (fans and louvers), air filtration systems, and source capture systems. Each method has specific advantages and disadvantages. It is not our purpose today to cover the pros and cons of each method, but one or more of the methods should be utilized to eliminate or control the dangerous contaminants introduced into the building through engine exhaust. The engine room pulling double-duty as PT and Dayroom.
The Transition Zone
Developing or expanding the Transition Zone is an important approach in both containing the contaminants and separating the occupants from the contaminants. Space will not allow us to discuss all items that can be addressed in the Transition Zone, but several ideas are easily identified. A dedicated Decontamination Area is paramount. The proper equipment that allows for the cleaning, treatment, and drying of all items that have been contaminated should be included in this Decon Area. Often the Decon Room includes, or is adjacent to the laundry area made for contaminated PPE or other articles. As previously implied, a dedicated PPE Room is not just about protecting PPE anymore.
This space accommodates the drying, off-gassing, and storage of potentially dangerous sources of contaminants. Proper drainage, heating, and ventilation should be provided.
If possible, a separate “dirty” Toilet/ Shower Room should be included in the Transition Zone. This will allow personnel contaminated from working in the Hot Zone access to a restroom facility without contaminating Toilet/Shower Rooms in the Living Areas of the station. It also allows a contaminated responder returning from a call the ability to shower
and change prior to entering the Cold Zone. Other items that should be considered for the
Transition Zone include;
Signage that prohibits PPE or other
gear beyond this zone
A boot cleaning station
A walk-off mat
Hand sinks or at least, hand sanitizer stations
Enclosed accommodations for the
ice machine and vehicle coolers
Easily accessible EMS Storage
All spaces within the Transition Zone should have a separated HVAC zone that does not allow return air into the Cold (Living) Zone heating and cooling system. Consideration should be given to sealing both ends of the Transition Zone, leading to the Hot and Cold Zones.
So, what can departments do to better contain the contaminants and separate occupants from the contaminants if it is still years before you can afford a new station or major renovations? Focus on the items that we’ve identified as the greatest hazards, along with the items that are easy (and inexpensive) to address. Look at how you are addressing vehicle exhaust. Some of the most common grant opportunities for fire departments cover vehicle exhaust systems. Evaluate how you clean, dry, and store PPE. Can you separate it away from all other zones in the station? Consider your decontamination spaces and practices, along with how they can be improved. Determine if your ice machine and vending machines are properly located and protected from dangerous exhaust. Make sure your physical training occurs outside of the Hot Zone. Install hand sinks, sanitizer stations, boot washes, walk-off mats, and signage at all doors leading into the Living Zone.
Conclusion
We all want emergency workers to go home safely to their families at the end of their shifts. But with the concerning statistics on fire fighter cancer rates, which are surfacing, we need to make every effort to assure a long, healthy life spent with their children
and grandchildren. Since 1988, Ken Newell, AIA, LEED AP BD+C, IAFC, has earned a national reputation for the design of Fire Stations that are functional, practical and budget conscious. He has been directly involved in the design of over 350 Fire Station,
EMS Stations and Public Safety Training Facility projects designed by Stewart-Cooper- Newell Architects. Since 2000, his practical approach to station design has led to him be a featured speaker at national Fire Station Conferences.